
New Tests Detect Deadly Lung Cancer Early
Early diagnosis is one of the best ways to beat cancer and there is good news on this front. Two new tests for lung cancer can detect this killer in time for treatment to be effective, thus giving patients a better chance for a cure.
In the first test, developed by Vadim Backman, professor of Biomedical Engineering at Northwestern University, Illinois USA, cell samples taken from inside an individual’s cheek are viewed through a specialized microscope. The microscope detects particular cellular changes, indicating whether lung cancer may be developing.
The second is a simple breath test! Exhaled breath contains thousands of volatile organic compounds (VOCs) that vary in composition and pattern. A subset of four VOCs have been discovered in the exhaled breath of lung cancer patients.
Cambridge, England-based Owlstone Medical developed a microchip sensor technology to measure VOCs in exhaled breath. This type of technology already exists. Co-founder and president of Owlstone Medical, Billy Boyle, says their smaller and less expensive device may become an in-office tool for doctors.
“We hope that breath analysis will allow us to diagnose patients with primary or recurrent lung cancer long before they suffer from symptoms, when we have more options for treating them, giving them the best chance for cure,” says cardiothoracic surgeon, Erin M. Schumer, MD, MPH, whose research on this technique was published in early 2016 in The Annals of Thoracic Surgery.
Smell Test Could Detect Prostate Cancer
A “smell” test promises to be an immediate and accurate diagnostic tool for prostate cancer. This may save thousands of lives and save thousands of men from having to undergo invasive investigations. The test is now in advanced clinical trials and is expected to be available to in late 2017.
Dr. Raj Persad, Consultant Urologist at Southmead Hospital, England, said: “If this test succeeds a full medical trial it will revolutionize diagnostics.
“Even with detailed biopsies there is a risk we may fail to detect prostate cancer in some cases.”
More than 1.1 million cases of prostate cancer were recorded globally in 2012, according to the World Cancer Research Fund International.

What’s Your Heart Attack Risk?
Imagine the day when a blood test could predict whether you are likely to have a heart attack within five years, thus allowing you and your medical practitioner to do everything possible to prevent such an event.
Well, another simple blood test, developed by researchers at the National Heart and Lung Institute, Imperial College London, promises to do just that.
If clinical trials are successful, instead of using age, sex, cholesterol and blood pressure levels and medical history to evaluate your risk of heart problems, the new test looks at protective antibodies that already exist in your system. These immune-system-produced antibodies, called IgG, seem to shield the body from a heart attack, even when cholesterol and blood pressure are high.
In the trial, those with the highest number of IgGs had a 58 percent lower risk of developing coronary heart disease or having heart attack. These individuals also had a 38 per cent lower chance of suffering a stroke during the five-year trial period.
Treatment Breakthrough for Breast Cancer
“Astonishing!” and “Ground breaking!” and “Game-changing potential!” is how breast cancer experts are describing the results from a recent trial.
Researchers from Cancer Research UK gave women with aggressive breast cancer a combination of two cancer-treating drugs: Herceptin (trastuzumab) and Tyverb (lapatinib). After 11 days of treatment with the drug combo, 17% of women saw their tumors shrink drastically. Even more impressive: Tumors completely disappeared in another 11% of women given both drugs.
In the trial, the researchers had been looking to see how the combined drug treatment affected tumors between diagnosis and surgery; the “unexpected” results were “dramatic”. Both drugs are current breast cancer treatments, so the combination therapy could be prescribed very soon—excellent news for some breast cancer patients.
Non-Invasive help for the partially blind
Until now, vision loss due to glaucoma or optic nerve damage has generally been considered irreversible. But a German clinical trial results published in June 2016 has demonstrated significant vision improvement in partially blind patients after 10 days of noninvasive, transorbital alternating current stimulation (ACS): This is when alternating currents of electricity are applied to the area of the brain that processes vision.
“ACS treatment is a safe and effective means to partially restore vision after optic nerve damage,” commented lead investigator Bernhard A. Sabel, PhD, of Otto-von-Guericke University of Magdeburg, Germany.
And more good news for those with low vision: A specialized miniature camera mounted onto their
eyeglasses, dramatically improves their ability to read.
The device recognizes text and reads it to the user who uses an earpiece, according to researchers with UC Davis Health System, California. The device can also be programmed to recognize faces and money and grocery items.
Blood Tests Accurately Detect Alzheimer’s
Like cancer, early diagnosis of Alzheimer’s disease can be of tremendous benefit to the patient. Two blood tests—developed separately and an ocean apart—can detect with an extremely high degree of accuracy if a person with mild cognitive impairment (MCI) is in the early stages of Alzheimer’s, or another cause of dementia.
Researchers at Rowan University in New Jersey, USA and at the Universities of Ruhr Bochum and Gottingen, Germany, both developed blood tests. More than 47 million people worldwide have dementia, and for the majority of them, their dementia is caused by Alzheimer’s.
This is a big advance as it offers many potential benefits for Alzheimer patients. It could allow specialists to slow the progression of the disease through lifestyle adjustments, medication and planned medical care. The German test has completed clinical trial, and further studies are now needed.
Stunning Recoveries Long After a Stroke
A 71-year-old wheelchair-bound stroke victim is walking again.
Scientists at California’s Stanford University School of Medicine have reported that seven of 18 stroke patients who agreed to undergo a trial therapy injecting stem cells into the damaged parts of their brains, have showed “stunning” results.
Gary Steinberg, the study’s lead author and chair of neurosurgery at Stanford, said in an interview that while he is cautious about “overselling” the results of such a small study, his team has been “stunned” that seven of the 18 patients experienced significant improvement in their abilities following treatment.
“Their recovery was not just a minimal recovery like someone who couldn’t move a thumb now being able to wiggle it. It was much more meaningful,” said Steinberg, who personally performed most of the surgeries.
Incredibly, the therapy worked for patients whose strokes had occurred between six months and three years previously. The new therapy essentially turns the adult brain back to an infant brain so that it can rebuilditself—something that was not thought possible until now.
The scientists believe the therapy could also work for traumatic brain injury and neurodegenerative conditions such as Alzheimer’s disease, Parkinson’s and Lou Gehrig’s Disease.
Nicholas Boulis, a neurosurgeon and researcher at Emory University, Georgia, USA, said, “There is certainly reason to be enthusiastic based on the magnitude of responses from these patients.”
Vaccine Coming To Fight Against Hospital Germs
Today we worry that we may get sicker when we’re in hospital than we were when admitted—and it’s no joke. Germs continue to flourish in hospitals, and C-difficile is one of the most prevalent and dangerous, especially for the elderly. But a vaccine may soon be available.
Scientists from the Max Planck Institute of Colloids and Interfaces, in Potsdam and the Freie Universität, Berlin, have developed a substance that elicits an immune response against the gut bacterium, Clostridium difficile.
The potential vaccine primes the immune system to recognize the pathogen itself, and produce antibodies to destroy it. The discovery may pave the way for developing inexpensive and effective vaccines and drugs against C. difficile. Other companies are also working on a vaccine, including Pfizer and Sanofi Pasteur.
Lighting Can Lighten the Pain for Migraine Sufferers
Green light gets the green light for migraine sufferers as researchers at Harvard University have found that low-intensity green light seems to reduce pain.
It’s been known for some time that light can trigger or increase pain for migraine sufferers: White, blue, red and amber light all increase migraine pain. But with the discovery that green reduces the pain, the team hopes that specially developed sunglasses that screen out all lightwaves except green will help.
Says Rami Burstein, PhD and Harvard professor of anethesia, “We were surprised to see that blue light was no more painful than white or amber or red, says Burstein. “They were all painful.”
But even more surprising was the finding that low intensities of green light lowered the volunteers’ suffering.
Electrical Stimulus Reduces Arthritis Pain
Clinical trials delivering electric current to the vagus nerve—which runs from our brain stem to our abdomen – have demonstrated that stimulating the vagus nerve significantly improved pain and swelling in patients with rheumatoid arthritis (RA).
RA is a chronic inflammatory disease that affects approximately three million people across continental
Europe. The findings were announced in July 2016 by Dutch and American researchers.
“These results support our ongoing development of bioelectronic medicines designed to improve the lives of people suffering from chronic inflammatory diseases and give healthcare providers new and potentially safer treatment alternatives at a much lower total cost for the healthcare system,” says Anthony Arnold, Chief Executive Officer of SetPoint Medical While focused on rheumatoid arthritis, the trial’s results may have implications for patients suffering from other inflammatory diseases, including Crohn’s, Parkinson’s, Alzheimer’s and others.

Unlocking memory
Health “Ah! That smells like the old days!” exclaims an old lady as she catches a whiff of a coffee substitute she remembers from her youth. Her companion points to a large pot on a radiator. It’s used for boiling nappies, she explains to their hostess, who is showing them round her home. But this is no ordinary home. And these are no ordinary visitors.
The ‘House of Memories’ is a replica of an apartment from the 1950s at Den Gamle By Museum in Aarhus, Denmark. It is intended for visitors living with Alzheimer’s and other forms of dementia.
The idea is to trigger memories—and early memories tend to be the best preserved and most easily recalled by association. So it is left to the sights and sounds to trigger recollections. Visitors leave noticeably lightened, and museum worker Henning Lindberg says he’s witnessed people talking for the first time in years and recalling stories their children have never heard.
Like all institutions, the house has to move with the times. There’s a plan to give it an upgrade soon—to the 1960s.
France acts on plastic
Environment The French love a picnic, and they love a glass of wine. But these pleasures can come at some cost to the environment. Every year, the nation throws away billions of non-biodegradable plastic goblets and other plastic utensils. As well as picknickers, vending machines and fast food restaurants are also culprits.
But now the French government has decided to ban sales of all single-use plastic plates, cutlery, cups and glasses from 2020, unless they are made of bio-sourced materials that can be broken down in a home composter.
Acid pollution declines
Ecology Danish researchers have discovered that man-made acid pollution of the atmosphere is almost back to pre-industrial levels.
For the first time, they were able to distinguish between man-made acids, caused mainly by fossil fuel consumption, and those produced by volcanic eruptions or forest fires. Production of the former reached its peak in the 1970s, but following clean air acts in Europe and the US, and effective industrial filtering methods, man-made acid pollution has now fallen to 1930s levels.
Heroes
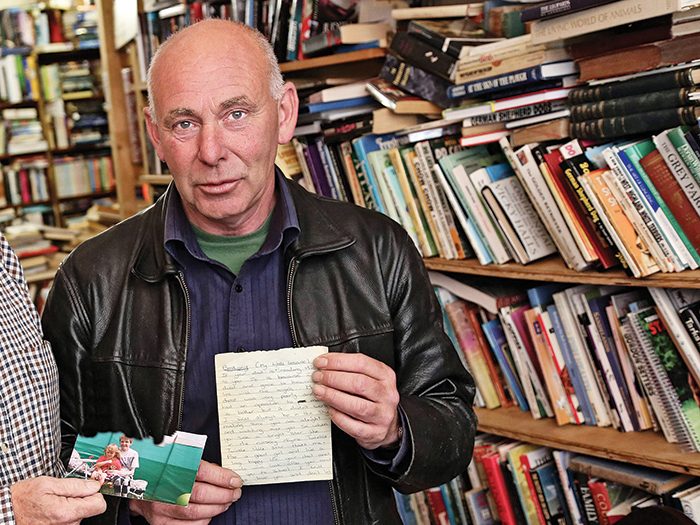
An Emotional Reunion Gordon Draper was sorting through some books in his secondhand bookstore in northeast England, when an envelope fell out. Inside was a letter and a photograph of a woman holding a small girl. It was addressed to “Bethany” and signed “Mam”. Draper realized it was a final letter from a dying mother to her daughter.
So he decided that he must track Bethany down. And that’s how Bethany Gash, now 21 and a mother herself, was reunited with the letter she had lost at the age of nine, five years after her mother died.
“I wanted to burst out crying,” she said. “The lengths he went to track me down, it was so overwhelming.”
Sources: Health: NPR, 13.9.2016 x.x.2016. Environment: Washington Post, 19.9.2016. Ecology: University of Copenhagen, 19.9.2016. Heroes: Washington Post, 9.9.2016

Most of us have experienced times where we overindulged on food. And that’s okay—the occasional Netflix-and-junk-food marathon feels good, even if we may regret the jumbo-sized bag of cheese doodles later.
Binge Eating Disorder isn’t like that. B.E.D. is a serious medical condition characterized by regular episodes of binge eating. It’s more than just overeating: People with the disorder feel like they lose control during a binge, which can cause feelings of distress, self-loathing and shame. There are several misconceptions about B.E.D., even though it’s the most common eating disorder—more so than anorexia and bulimia combined. Here, we clear up some common myths about the disorder.
Myth: Binge Eating Disorder is a Choice
Real Talk: For people with B.E.D., bingeing is not a “lifestyle choice,” or a “phase.” It is a mental illness associated with mood disorders, anxiety and depression. The exact cause of B.E.D. is unknown, but research suggests that family history and brain chemicals may be involved. Stressful life events could also play a role in the disorder.
Myth: Only Obese Individuals Suffer from B.E.D.
Real Talk: B.E.D. is associated with increased weight, but the disorder affects people of all shapes and sizes; normal-weight, overweight and obese individuals can have B.E.D. One U.S. survey even found that the majority of adults with B.E.D. are normal-weight or overweight. In the study, 55% of participants had a BMI of 30 or lower, versus the 45% who had a BMI over 30, putting them in the obese range.
Myth: B.E.D. Only Affects Women
Real Talk: It’s a widely-held belief that only women and girls suffer from eating disorders, but that simply isn’t true. Binge Eating Disorder affects both men and women. It’s estimated that approximately twice as many women are affected as men: A study by researchers at Harvard University found that lifetime prevalence of B.E.D. was 3.5% in women and 2.0% in men.
This myth about eating disorders being exclusive to women can make it more challenging for men to seek treatment. They may not come forward because of embarrassment, or they may not even recognize that anything is wrong.
Myth: Recovery is Not Possible
Real Talk: There are several management options available to people struggling with B.E.D. One widely-studied treatment is cognitive behavioural therapy (CBT), which encourages individuals to regulate their eating habits through goal setting and self-monitoring strategies. These therapies can help reduce the frequency of binges: In a study of 125 obese patients with B.E.D., published in the Journal of Consulting and Clinical Psychology, just over half of the participants went into binge-eating remission one year after using CBT.
Other treatment options include nutritional counselling and medication. If you think you may have B.E.D., start the conversation with your family doctor. You may not feel comfortable talking about it, but asking for help is the first step to recovery.

As the grey October light fades away, two dozen people mill about in a courtyard in Winnipeg’s North End. They clutch Styrofoam cups of coffee and carry backpacks filled with supplies: first-aid kits, for instance, or fruit and extra mittens. (Here are six inspired ways to put Styrofoam to good use around the house.)
At the head: broad-shouldered 48-year-old James Favel, who divides those assembled into women-led crews of five. “Pitter patter, let’s get at ‘er,” he then commands, and the groups fan out. Their two-way radios crackle to life, and the beams of their flashlights bob along the pavement.
This is how most nights begin for Bear Clan Patrol Inc. Five times a week, its volunteers hit the streets, their yellow vests a new fixture in this corner of town, which has long wrestled with some of the highest crime and poverty rates in the city. Their nightly mission is open-minded, an ad hoc mixture of social outreach and anti-violence intervention.
A year and a half ago, Winnipeg was still reeling from the August 2014 murder of Tina Fontaine, a 15-year-old Anishinabe girl. Favel, who chairs a North End residents’ association, was eager to set up something to help protect women in the area.
In this, he was inspired by the work of a local young organizer named Michael Champagne, who spearheads a series of weekly community meetings designed to push back at violence. “He showed me that it can be done,” says Favel.
On one Thursday in the fall of 2016, Bear Clan members were first on the scene to assist a man who had lost two of his fingers in a machete attack. The next evening, the patrol defused a street fight and raced to help a young mother after an estranged ex-partner forced his way inside her apartment.
It was an unusually hectic couple of nights. Even before the Friday shift began, one member spotted two used needles on the ground. Sometimes they find baggies of meth. But often the patrol is uneventful – the crew greets everyone they pass and pause to chat or hand out snacks.
The original incarnation of Bear Clan, co-founded by the late indigenous advocate Larry Morrissette, patrolled the neighbourhood in the 1990s but eventually fizzled out. The initiative was officially revived in 2015, with Morrissette’s blessing.
Under Favel’s leadership, Bear Clan 2.0 has built working relationships with the Winnipeg Police Service. It has also sparked a spinoff, Mama Bear Clan, in the adjacent neighbourhood of North Point Douglas. There are plans to add a youth patrol.
The demands of organizing have become so great that Favel has left both his job as a trucker and a part-time gig at a North End halfway house. To make ends meet, he has cobbled together community grants while he searches for stable funding. He doesn’t mind, though. “I was never fulfilled by trucking like I am with this work,” he says. “Seeing the community come together and seeing the smiles on people’s faces when you give something to eat, well, not to be corny, but it feels good.”
Through Bear Clan, Winnipeg is united. Volunteers who show up to patrol come from varying backgrounds. They include grandmothers, army veterans, doctors, ex-bikers who have served prison time and residents of the city’s wealthier suburbs. Others have no permanent home. Twenty-year-old Meagan Owen had spent much of 2015 struggling with poverty and addiction when patrolling Bear Clan members offered to help her secure housing and employment. At first, she resisted. “I was kind of apprehensive,” she says, “but all the people I’ve talked to went through it – the addictions and the struggles.”
Now Owen is reaching out to others by regularly joining the patrol. In early November, she was preparing to enter an addiction treatment program and hoped to secure work as a chef. “I’m feeling like I accomplished something,” she says. “it’s productive.”
Reader’s Digest: You’ve been a family doctor since 2005. Then, in 2014, a video of you defending Canada’s medicare at a U.S. senate hearing went viral. You say that sparked your new book, Better Now. How?
Danielle Martin: Millions of people watched me battling it out with a Republican senator, and there was a massive influx of support from Canadians that made me realize how committed they are to our health care system. It gave me hope that we can actually make positive changes here.
You argue that too many Canadians still don’t get the medical treatment they need. What frustrates you the most?
It bothers me, as both a doctor and a patient, that two people with the same condition, in the same community, can have very different experiences. Sometimes it works well; other times it really doesn’t.
Your grandfather, who immigrated to Montreal from Cairo in 1951, died of arterial disease in 1966. His ill health devastated your family, and if he’d had access to medicare, he might have lived a long life. Is that why you became an activist?
He’s why I grew up in a household where we believed access to care should be based on need, not ability to pay. The idea that we all have an obligation to make things better for people was a reigning philosophy in my home, and a lot of that came from my mom – her early childhood experience shaped who I am.
Your mother must be proud.
When she’s not driven insane by me.
In the book, you describe many patients who’ve inspired you to fight for more equitable access to care. Does anyone stand out?
Ahmed, the taxi driver who can’t afford medicine to control his blood pressure and diabetes. One in 10 Canadians aren’t taking a drug they’ve been prescribed because of the cost. Modern medicine is powerful, but if people can’t afford it, it doesn’t do much good.
You offer up six recommendations to fix the system. Which one would have the biggest, most immediate impact for patients like Ahmed?
We pay way too much for prescription meds. If we brought the necessary ones under medicare, we could bargain for better prices. Short of paying for Ahmed’s pills, I can’t do anything to make his situation better on my own. The solution he needs can only be implemented through changes to public policy.
It must be disheartening to have patients you can’t help.
I can sit at home and be sad or I can do something. That’s what this book is about. I’m trying to start a national conversation about the concrete, achievable things we can do to make things better.
Can average Canadians take steps to improve the system?
To change policy, each citizen has to write a letter to their MP or raise the issues during election campaigns. But we can also have an impact by asking questions before agreeing to tests or procedures. As patients, we can say, “Hang on – are we sure this is actually going to improve my health?” Just by reducing unnecessary testing, we’d see an improvement in the system right away.
Better Now is available on Jan. 10.