What You Need To Know About Adult-Onset Allergies

Adult-onset allergies can strike at any time—even if you've never had one before. We chatted with the experts to find out potential triggers and how to take preventative action.
The world is full of allergens from food, bugs, pollen, latex, drugs, mould and animals—for a start. Many of us assume that our susceptibility to them develops only during childhood, so if you’re allergy-free in your 20s, you’re in the clear. But researchers are discovering that it’s possible for adults of all ages to acquire allergies—even if they’ve never had one before.
In 2019, for the very first systematic study of allergies in adulthood, the Center for Food Allergy & Asthma Research (CFAAR) surveyed approximately 40,000 people across the United States and found that one in 10 were food-allergic. Half of those people, the survey revealed, developed at least one of their allergies after the age of 18. “We were very surprised by the results,” says Ruchi Gupta, CFAAR’s director. Her team had long suspected, based on anecdotal evidence, that rates of adult-onset food allergies were rising, but they didn’t expect the number to be so high.
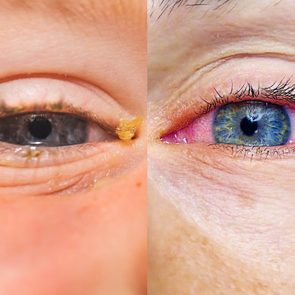
While CFAAR’s study primarily looked at food allergies, it also provides insight into other types since people with one type tend to have others. That’s because our bodies react in a similar way to them all: after exposure to a benign substance that the immune system mistakenly sees as harmful, antibodies cause cells to release chemicals such as histamine, which triggers inflammation. This is the body’s way of protecting itself from potentially dangerous substances. But as a side effect, histamine brings on hives, watery eyes, nasal congestion and, for some severe cases, a drop in blood pressure, leading to anaphylactic shock.
While scientists don’t know for sure what causes new allergies to form in adults, Gupta’s team has identified some likely triggers. Exposure to a new environment could introduce new allergens to your system—which is why someone who just moved to Seattle, where alder trees are common, might develop a new allergy to alder pollen, for example. People experiencing a hit to the immune system (such as a viral illness) or going through hormonal changes (such as in puberty or menopause) may also be at higher risk of developing new allergies, since their body’s defence systems may already be weakened.
Unfortunately, it’s not always easy to discern which allergy you have or whether you really have one. According to Gupta, people can easily mistake food poisoning and food intolerance for allergies. To identify a real one, doctors might conduct a blood test, a pinprick test (which inserts a small amount of an allergen into the skin) or an “oral food challenge,” where a patient is supervised by a doctor while they consume a particular food.
There’s no one-size-fits-all treatment for allergies, but antihistamine medication serves as a helpful over-the-counter treatment for mild symptoms. To address environmental allergies, doctors can prescribe a regular series of injections that gradually expose and habituate the immune system to larger doses of the allergen. New treatments, such as oral immunotherapy (which is the same basic idea but through ingestion), are an option for food allergies.
Gupta’s research is at an early stage, and it’s still unclear whether adult-onset allergies eventually resolve or persist for life. That’s why the best strategy may be preventative, says Christopher Warren, a researcher at CFAAR: to avoid developing allergies, a good bet is to expose ourselves to allergens regularly, so our body is acquainted with the substances. Children and adults should be eating a healthy, diverse diet that includes the most typical allergens, such as shellfish, milk and peanuts. As for environmental allergies, as long as we are reasonably safe, one of the best things we can do is to keep playing in the dirt.
Now that you know the latest research on adult-onset allergies, find out which four skin changes you should never ignore.