Anxiety Is On the Rise During COVID-19. Here’s What You Can Do to Help Ease It
Compounding crises have made everyone anxious, but how do you know if you’ve slipped into a more serious disorder—and what do you do about it?
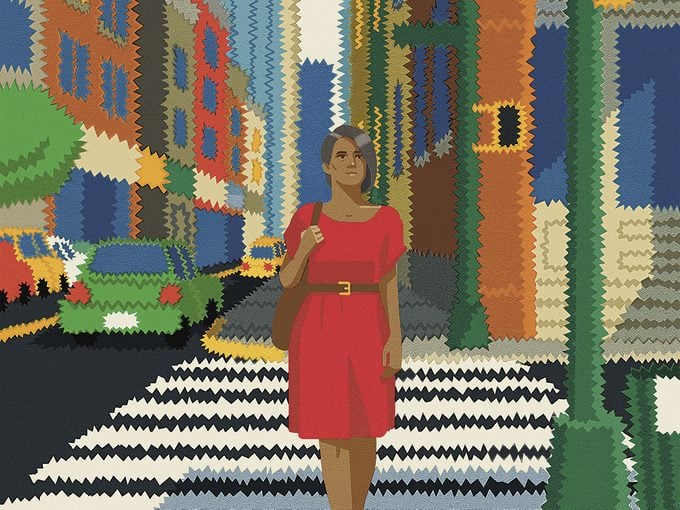
Five years ago, Meredith Arthur, a 45-year-old San Francisco employee of the social media company Pinterest, arrived at a neurologist appointment in a distraught state. She spoke a mile a minute, rattling through her extensive research on the vagus cranial nerve and explaining why she thought it might hold clues to her crippling shoulder and neck pain, frequent dizziness and nausea and chronic migraines. “I was presenting my inexpert case to an expert, and she stopped me and said, ‘I know what’s wrong. You have generalized anxiety disorder.’”
For Arthur, the diagnosis was a shock. She had been so focused on her debilitating physical symptoms that she hadn’t considered that they could be linked to her mental health. But almost immediately, it clicked.
“My brain was always in overdrive, from early childhood,” Arthur recalls. “I always wanted to work really hard all the time and solve everything.”
She would have never described herself as a worrier, however, and certainly didn’t connect her perfectionism to anxiety or its impact on her body. But in fact, physical discomfort (like stomach and chest pain, feeling restless or irritable, sleep problems, fatigue and muscle aches) is most often what drives people with anxiety to seek treatment, not distressing thoughts.
“The diagnosis changed everything,” says Arthur. “It’s like somebody picked me up off the earth, turned me around 180 degrees and put me back down. It was the same world, but everything looked a little different.”
Arthur is one of the 44 million North American adults who experience an anxiety disorder—the most common form of mental illness—every year. But beyond serious cases, anxiety is something that touches everyone to varying degrees. Typically, it’s intermittent and brought on by a stressful or traumatic event. The core features of anxiety are excessive fear and worry—followed by extreme problem solving, in Arthur’s case—and one of the major underlying factors is a feeling of uncertainty about situations that occur in daily life.
Enter big, bad 2021. These are exceedingly anxious times due to the unholy combination of economic precariousness, social unrest, political volatility, environmental catastrophes (pause: deep breath) and the COVID-19 pandemic. But an individualized, holistic approach to managing anxiety—including lifestyle tweaks, medication, mindfulness exercises and, to begin with, acceptance—will ensure it doesn’t rule your life.
What Anxiety Does to Your Body
Anxiety is part of your body’s stress-response system—and it’s uncomfortable, overwhelming and sometimes plain confusing.
“I describe anxiety as a future-oriented emotional response to a perceived threat,” says Dr. Joel Minden, a clinical psychologist and the author of Show Your Anxiety Who’s Boss. “We anticipate that something bad will happen. Maybe we have evidence for thinking that. Maybe we don’t. But we have a belief that something catastrophic might occur.”
Almost immediately after that, Minden says, your sympathetic nervous system, which controls involuntary processes like breathing and heart rate, kicks into high gear. This leads your adrenal glands to release adrenalin and cortisol, two of the crucial hormones driving your body’s fight-freeze-or-flight response, which prompt anxiety’s physical symptoms. Your heart races, your blood pressure rises, your pupils dilate, you get short of breath and you break out into clammy sweats.
Meanwhile, cortisol curbs functions that your brain considers nonessential: it alters immune-system responses and suppresses the digestive system, the reproductive system and growth processes. This was helpful for our ancestors trying to outrun a sabre-toothed tiger, but not so much when you walk past someone in a grocery store and, even though you’re both wearing masks, can’t stop ruminating for days afterward about whether you might have caught COVID-19 when they coughed.
“The physiological sensations you get make sense when you’re in danger,” says Dr. Melisa Robichaud, a psychologist and clinical instructor in the University of British Columbia’s psychiatry department. “But they feel odd and sometimes quite scary when there’s no physical threat.”
Everyday Anxiety or an Anxiety Disorder?
For Arthur, chronic physical pain and discomfort were the most powerful manifestations of her disorder, but anxiety can show itself in many ways. You might perceive something as threatening, even when it isn’t, or go to great lengths to avoid uncomfortable situations. You might constantly overthink plans or spend all of your time creating solutions to worst-case scenarios that are unlikely to happen. Maybe you’re indecisive and fear making the wrong decision. Or you might find yourself unable to relax and feel restless and keyed up.
Often, those symptoms last only as long as a certain situation or problem is present. (You may feel nervous about flying, but you do it and the feeling fades when the wheels touch down.) But sometimes anxiety can tip into a chronic anxiety disorder. These include generalized anxiety disorder, but also panic disorder, social anxiety disorder, obsessive-compulsive disorder, post-traumatic-stress disorder and phobias. People with an anxiety disorder can also suffer from depression—and in fact, some estimates show that 60 per cent of those with anxiety will also have symptoms of depression.
The distinction between circumstantial or temporary anxiety and a more severe case isn’t always easy to make, says clinical psychologist Dr. David Carbonell, founder of the Anxiety Treatment Center in Chicago.
“There isn’t a blood test for anxiety. At some point, everybody experiences it,” he says. “It becomes a disorder when it interferes with your behavioural choices and your ability to do as you wish in life.”
For instance, that point could be when your job requires you to fly, but you’re too anxious to even make it as far as the airport, which ultimately puts your livelihood in jeopardy. Or, more generally, when you find that anxious feelings last for a long time, beyond when a problem has passed or been resolved, and they seem to jump from one situation to the next without relief.
Despite the fact that chronic anxiety is very manageable with professional help—and some combination of medication, therapy and lifestyle adjustments—only about 37 per cent of affected people receive treatment of any kind. “I always say that I have a really good job because I specialize in treating people who have anxiety disorders,” says Robichaud, “and by and large, most everyone I see gets better.”
How to Treat an Anxiety Disorder
1. Accept It
Just like happiness and sadness, anxiety is part of everyone’s lived experience—but it’s not always tolerated as such.
“People spend too much time and effort on trying to control anxiety,” says Minden. “I encourage them to remember that anxiety is a normal emotional response.” If you try to banish it, he adds, all you’re doing is putting it more at the forefront of your mind. But if you accept anxiety as part of life, you can learn to relate to it with self-compassion or even with humour. This is a cornerstone of acceptance and commitment therapy (ACT), which has been gaining clinical validation, including by the American Psychological Association.
ACT guides people to see their unpleasant emotions as just feelings and to accept that parts of life are hard. Practitioners encourage patients to begin a dialogue with anxious thoughts, examining their causes while also keeping in mind their personal goals and values. Although anxious thoughts shouldn’t be completely suppressed, sufferers can deliberately not allow anxiety to decide what gets their attention or turn them away from what they want to do and who they want to be.
This way of relating to anxiety has been a powerful strategy for John Bateman, the 52-year-old host of the podcast Our Anxiety Stories. When negative or irrational thoughts arise, he acknowledges them but doesn’t let them drive his decisions.
Over the years, Bateman has noticed that if he acquiesces to his thoughts, they don’t go away but dramatically increase. But if he recognizes them for what they are, just a passing thought and not a fact that needs to be acted on, they diminish. Since beginning to train his brain to think in this new way eight years ago, he’s noticed that the negative thought patterns have lessened. “I discovered that my brain is this amazing, elastic thing,” he says.
2. Be Curious About It
After acceptance, a mindfulness approach to anxiety can be useful, especially when you’re cycling through anxious thoughts and are unable to think clearly or rationally.
In his book Unwinding Anxiety, psychiatrist and neuroscientist Dr. Judson Brewer recommends paying attention to the body sensations, thoughts and emotions that come as a result of feeling anxious or worried. When we notice and name the physical sensations that are arising in our bodies (my face feels hot and flushed; my breathing is shallow; my heart is beating quickly; I feel sweat prickling my underarms), we are already less caught up in it, simply through that act of observation, writes Brewer.
Many mindfulness training apps can provide you with help, including one that Brewer developed in his lab at Brown University and shares a name with his book. After three months of using the app, a test group reported a 57 per cent reduction in their anxiety.
Understanding exactly what was happening inside her body and bringing her awareness to it was an empowering tool for Arthur. When she’d notice the shaky feeling in her chest or belly that radiated out to her hands and down her legs, she knew that meant adrenalin had been released. And by noting these changes as an observer, her “thinking brain” could take over from her immediate fight-freeze-flight reaction to an anxious moment—and as she began processing what just happened, her symptoms became less acute and threatening. She pictured the hormones hitting her body the same way an ocean wave hits the beach. The beach can’t fight the wave, but it remains steady and allows the wave to wash over and fall back.
3. Make Lifestyle Adjustments
Learning to live with anxiety is an individual process, and one that requires trial and error to get just right. While acceptance is the first and most important step to take, some lifestyle changes have been proven to take the edge off, as well.
Since fatigue and increased tension and stress leave us more vulnerable to anxiety, a well-balanced diet, adequate rest and, especially, regular exercise can help us manage it better. In one study, researchers showed that regular vigorous workouts lead people to be 25 per cent less likely to develop an anxiety disorder or depression over the next five years.
Meredith Arthur’s toolkit consists of medication—a prescription SSRI antidepressant—and regular meditation. She also shares her experiences on and edits stories about mental illness for the web platform Medium and recently wrote Get Out of My Head, an illustrated guide on how to understand anxiety and learn to navigate problems without overthinking.
Openly discussing the condition with an online community and readers has transformed her relationship with anxiety. “I’m learning to live in harmony, as much as possible, with this thing that is a part of me,” she says. “It’s not always pleasant, but I’m learning to accept and, as much as I can, take care of my anxiety.”

There’s No Shame in Taking Medication
Many people avoid taking, or even looking into, medication for anxiety because of the stigmas associated with psychiatric drugs. They may worry about dangerous side effects, that they’ll become dependent on them or that loved ones will see them as weak or flawed.
But the fact is, modern pharmacological treatments for anxiety disorders are safer and produce fewer side effects than they did 30 years ago. At the same time, attitudes toward mental illnesses are improving: a 2019 survey by the American Psychological Association found that 87 per cent of adults agreed that having a mental-health disorder is nothing to be ashamed of.
If you’re ready to explore medication, Dr. Debra Kissen, CEO of Light on Anxiety CBT Treatment Center, suggests talking to a primary care doctor, who can prescribe the medications most commonly taken for anxiety.
Selective serotonin reuptake inhibitors (SSRIs) are considered a good starting medication for many forms of anxiety. Serotonin is a neurotransmitter that plays a role in feelings of well-being and happiness, as well as thinking, memory, sleep, digestion and circulation. SSRIs increase levels of serotonin in the brain and are considered non-addictive and safe for long-term use.
Another choice is benzodiazepines, or “benzos,” which strengthen the effect of the neurotransmitter GABA—the primary inhibitory (“turn off”) signaller in the brain. Benzos are fast-acting and don’t stay in your system for long, but they are considered unsafe for continuous use and are potentially addictive.
Kissen believes therapy is still crucial because the gains are hardwired into your brain. For moderate to severe anxiety, combining therapy with medication is generally the most impactful. “It’s a one-two punch where the medication is setting up the environment of your brain to make the most rapid gains as you’re doing the work of learning new ways of looking at situations,” says Kissen.
Next, check out these tips that will help you live to 100!






