
What’s Wrong With Me?
The patient: Benjamin*, a six-year-old boy
The symptoms: Hives and anaphylaxis
The doctor: Dr. Yuval Tal, head of the Clinical Immunology and Allergy Unit at Hadassah Medical Center in Jerusalem, Israel
In infancy, Benjamin Linderman frequently battled lung infections and breathing problems. He was diagnosed with asthma by the age of two. Symptoms of that condition can sometimes be triggered by food allergies, and since an older sibling experienced just that, Benjamin’s parents sought testing. Results showed their son was allergic to dairy, potatoes and a few other foods. Once these were eliminated from his diet, his asthma symptoms and lung infections subsided.

Breaking Out
But in 2011, when Benjamin was four, a new mystery appeared: the boy began getting intensely itchy rashes on his neck, arms and other parts of his body. At first, his parents thought their son might be reacting to an antibiotic he was on. Another possibility was an irritant like laundry detergent. The rashes typically vanished within hours, however, which meant they were urticaria, or hives. About one in five people experiences hives occasionally, but for Benjamin they soon became a daily issue.
His family noticed the reactions seemed the worst—particularly on exposed skin—whenever Benjamin had been playing outside. Could he be reacting to sunlight? Solar urticaria is a rare allergic response, accounting for probably only one per cent of chronic hives cases, in which exposure to UV light causes certain cells in the skin to release histamine.
Benjamin’s long-time allergist was baffled. “He said, ‘I’ve heard of this, but it couldn’t possibly be, it’s so incredibly rare,’” recalls Benjamin’s dad, Matthew Linderman.
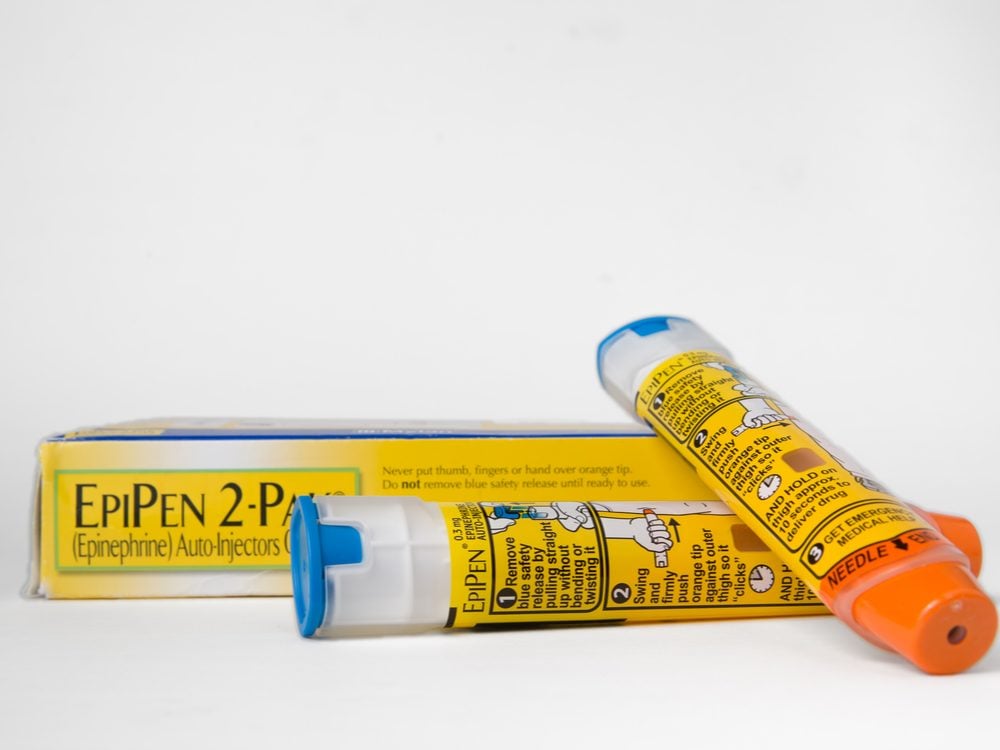
They were referred to a dermatologist at Jerusalem’s Hadassah Medical Center, who recommended keeping Benjamin’s skin covered and using a broad-spectrum sunscreen all over his body. But Benjamin got steadily worse. The reactions developed more quickly and took more time to settle down. He started swelling around his lips, and carried an EpiPen.
His parents began dressing him in long, dark clothes, and he didn’t go on class trips. These changes helped temper the rashes but, confoundingly, didn’t stop them altogether.
Meanwhile, another Hadassah dermatologist proposed light laboratory testing, in which a lamp shines lights of various wavelengths on different areas of skin, and pinpoints exactly which kind the patient is allergic to.
Learn how to tell the difference between common skin conditions.
“He’s taught a lot of people about how to cope with challenges in life.”
To everyone’s surprise, Benjamin reacted to all visible light—including that from indoor bulbs. This explained why sunscreen, which blocks only invisible UV rays, hadn’t helped.
Despite having to wear long clothes on even the most sweltering of days, Benjamin rarely complained, says his dad. “He’s taught a lot of people about how to cope with challenges in life.”
The family figured they could manage in this way, but one September evening when Benjamin was six, it became clear that was no longer the case. They’d celebrated the Jewish holiday Simchat Torah at a synagogue they didn’t normally attend. “We were surprised by how bright it was inside,” says Linderman. Once home, Benjamin began feeling unwell, then suddenly had trouble breathing. He was in anaphylactic shock. His frightened parents quickly administered the EpiPen and called an ambulance. Benjamin was rushed to the hospital, where a dark room was prepared for him, and the reaction was controlled with medications.
“Solar urticaria, in almost all cases, doesn’t endanger the person in any way. It’s just annoying,” says Dr. Yuval Tal, an immunologist at Hadassah. “Ben was different. He had a systemic response, which is extremely rare.”

A Real Breakthrough
Tal met with the family to explore new ideas. There was an immunosuppressive drug that had been helpful for some people with the condition, but the potential side effects (high blood pressure and impaired kidney function, among others) were too harsh for a young child. Attempting to desensitize Benjamin to light by gradually increasing his exposure to it might work, but it would be time-consuming and the benefits could wear off. Tal remembered that a colleague of his in Germany had recently been experimenting with omalizumab, an asthma medication for adults, to treat light allergies. No doctor had ever given the drug to a child, but Tal and Benjamin’s parents agreed it was worth trying.
“We had essentially no choice,” says Tal, who started by administering a low dose and carefully monitoring the child for a bad reaction. “I was frantic when I injected him. I practically tied the boy to my leg and walked with him for the entire day!” Although Benjamin tolerated the drug well, he didn’t improve. But after he was given a higher dose two weeks later, he wasn’t quite as itchy and swollen. It was the first real breakthrough since the onset of his light allergy. The dose was increased two more times, until his symptoms all but disappeared.
Discover the strange symptoms that can signal a serious disease.

A New Life
Five years later, 12-year-old Benjamin has settled into a regimen of injections every three weeks. Although his father still sees symptoms near the end of a treatment cycle, he says it’s nothing compared to what Benjamin used to suffer through: “He can now walk around in shorts and a T-shirt, and he plays games with the kids at school.”
Benjamin’s parents are forever grateful to the doctors at Hadassah. “They have done an incredible job in turning our little boy’s life around,” Linderman says. “And they stepped outside the box to make that happen.”
Next, check out the 50+ health symptoms you should never ignore.