This Man’s Medical Nightmare Will Make You Think Twice About How You Dress Your Bed
No one thought to draw a connection between his severe breathlessness and a recent purchase...
Martin Taylor, a 42-year-old software engineer by day, plays lead guitar in a local band in Aberdeen, Scotland. In September 2016, while helping his bandmates unload heavy equipment before a gig, he felt suddenly light-headed. He shrugged it off, but the sensation worsened over the next few weeks. Taylor felt increasingly breathless and tired that autumn. Meanwhile, his appetite dwindled. And though he’d try to get a good sleep, he’d frequently wake up during the night feeling light-headed.
Then one evening in November, while Taylor was setting up band equipment at a wedding, he had a bad dizzy spell. “I almost passed out,” he recalls. One of his bandmates grabbed him before he dropped to the ground. Finally, he made an appointment with a GP at a nearby medical practice.
The doctor thought Taylor had a minor chest infection that would pass, but Taylor only felt more wretched as the days went by. He returned and saw a different GP, who ordered a chest X-ray to look for any problems like bronchitis, pneumonia or even a tumour. The report was normal.
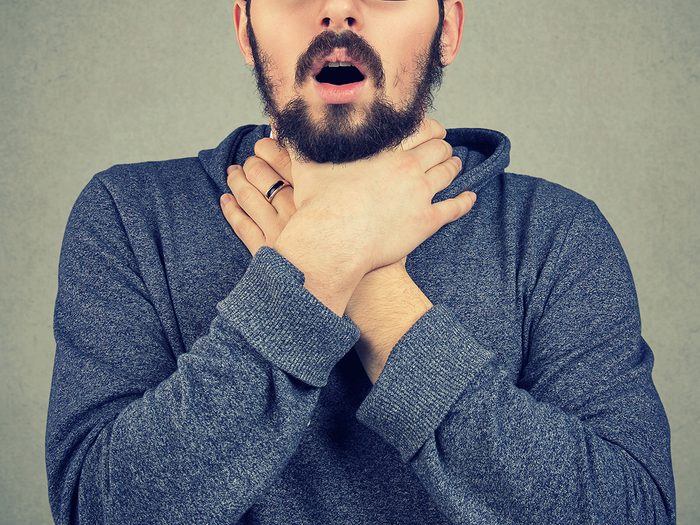
Gasping For Breath
By December, Taylor was too sick to go to work or band gigs. He slept around the clock and felt breathless at the slightest effort. Heading upstairs to rest took an agonizingly long time. “After a few steps, I would be totally winded,” he says. At night, he felt like he was suffocating and couldn’t get enough air into his lungs. Mornings, after Taylor’s wife left for work, his young daughter would carry up his tea or toast to him in bed. He says ruefully, “As a parent, you don’t expect to be looked after by your eight-year-old.”
At the same time, Taylor’s lack of appetite had caused him to lose more than 15 pounds. Desperate, he made an appointment with a third doctor at the same medical practice. This GP asked Taylor to walk rapidly through the corridors. Taylor gasped for breath. He clipped an oximeter onto Taylor’s finger to measure his blood oxygen. A normal range is above 95 per cent; Taylor’s was below 80.
“This Isn’t Normal…”
The doctor called his colleague, Dr. Owen Dempsey, a chest physician at Aberdeen Royal Infirmary, emailing him Taylor’s supposedly normal X-ray. “I clicked on the image as we were chatting,” says Dempsey. “I remember saying, ‘This isn’t normal.’ It was subtly abnormal.” Taylor’s lungs were faintly shadowed with grey, as though covered in a veil. A radiologist could easily mistake that for a slightly underexposed picture. Dempsey realized it could mean air was being displaced by something else, like fluid from inflammation.
Lung inflammation has numerous causes, including pneumonia or the presence of an autoimmune disease. Occasionally, it’s a sign of hypersensitivity pneumonitis (HP), an allergic-type reaction to something that’s been inhaled repeatedly, such as industrial chemicals, moulds or other irritants. HP is reported in only a couple of people for every 100,000, but researchers suggest it’s most certainly underdiagnosed. Says Dempsey: “The lungs are filtering thousands of litres of air a day. In a way, it’s surprising we don’t have more reactions than we do to things in the environment.”
Dempsey phoned Taylor at home. Partway through the call, Taylor had to pause to turn off the stove; when he returned from the kitchen, he was so out of breath he could barely speak. That made an impression on Dempsey. “A man his age shouldn’t be breathing as though he’s run a marathon, just from walking around his home.”

Identifying the Trigger
The doctor peppered him with questions. Hundreds of allergens are known to cause HP, but they’re often obscure, like unseen mould inside a wind instrument, or popcorn dust in a factory that produces the snack—and there’s no way to test for all of them at once. “In many cases, we can’t identify the trigger,” says Dempsey. “That’s frustrating, because the management of this illness is to eliminate the trigger.” He asked Taylor about birds, since a common type of HP is a reaction to the waxy, water-repellent coating on feathers. The problem is mainly seen in pigeon breeders and owners of pet budgies. Taylor didn’t keep any birds. But Dempsey went one step further, asking about feather bedding.
That’s when Taylor mentioned a new duvet and pillows he’d had since late summer. Although he and his wife had used feather duvets for years, this was the first time his pillow had been filled with feathers. “I sleep face down, so I had my face buried in it,” he says.
Dempsey recommended he replace the bedding immediately. He also prescribed steroids to reduce inflammation. Taylor was willing to try anything. “I’d been gradually feeling worse for so long, with no end in sight to the misery.”
A Miraculous Recovery
After a couple of nights with a new pillow, Taylor felt slightly less sick. He started the steroids a week later, and within two days his symptoms were completely gone. “It was euphoria,” he recalls. “I felt brand new again.” A lung CT scan confirmed the presence of those grey areas, and blood tests showed high exposure to bird proteins. Had Taylor continued using his feather pillow, he could have developed permanent scarring in his lungs.
Taylor, who was able to wean off the steroids, admits it took him a while to appreciate just how unusual his experience was. “Dr. Dempsey says I’m this special case. For the longest time, I thought he said that to all his patients—just to make them feel they were in good hands!”
Next, read the incredible story of how a woman’s x-ray revealed the reason behind a lifetime of stomach pain.






