
Your body’s defense system
Many times, a fever can be a sign that your immune system is functioning well. Your body heats up because it senses a foreign invader: “Bacterial, viral, or something else that’s not supposed to be there,” says Deborah Nunziato-Ghobashy, DO, family medicine physician at Scarsdale Medical Group.
“The hypothalamus in the brain controls your body temperature and raises it to kill off anything that could be invading your body,” she explains. “All those bacteria and viruses prefer a cozy 37-degree environment to keep on replicating. Once it’s higher, it’s too hot for them and they start to die off.”

Persistant fever
A fever is usually a sign that your immune system is busy at work fighting off an illness. But if you’re still running a temperature after three days, you should see your doctor.
“A fever with no obvious origin that persists despite the appropriate use of traditional fever-lowering agents—like acetaminophen, naproxen, ibuprofen, or aspirin—is concerning,” says Gary LeRoy, MD, a family physician in Dayton, Ohio and president of the American Academy of Family Physicians.
That’s especially true if you’ve been exposed to the coronavirus (fever is the most common symptom of coronavirus). A study published in The New England Journal of Medicine found that 44 percent of almost 1100 patients hospitalized with coronavirus in China had a fever when they first arrived at a healthcare facility.
“A persistent fever of 38 degrees or higher associated with a history of possible COVID-19 exposure should raise suspicion,” says Dr. LeRoy. “An episode of sudden confusion, agitation, or mental status changes in a young to middle-aged adult is also concerning.” (Here are 10 signs you may have already had COVID-19.)
Other physical signs requiring urgent attention, he says, are fevers accompanied by:
- Trouble breathing
- Persistent pain or pressure in the chest
- Inability to wake or stay awake
- Bluish lips or face
- Rapid pulse/heartbeat

Pain on the lower right side of your belly
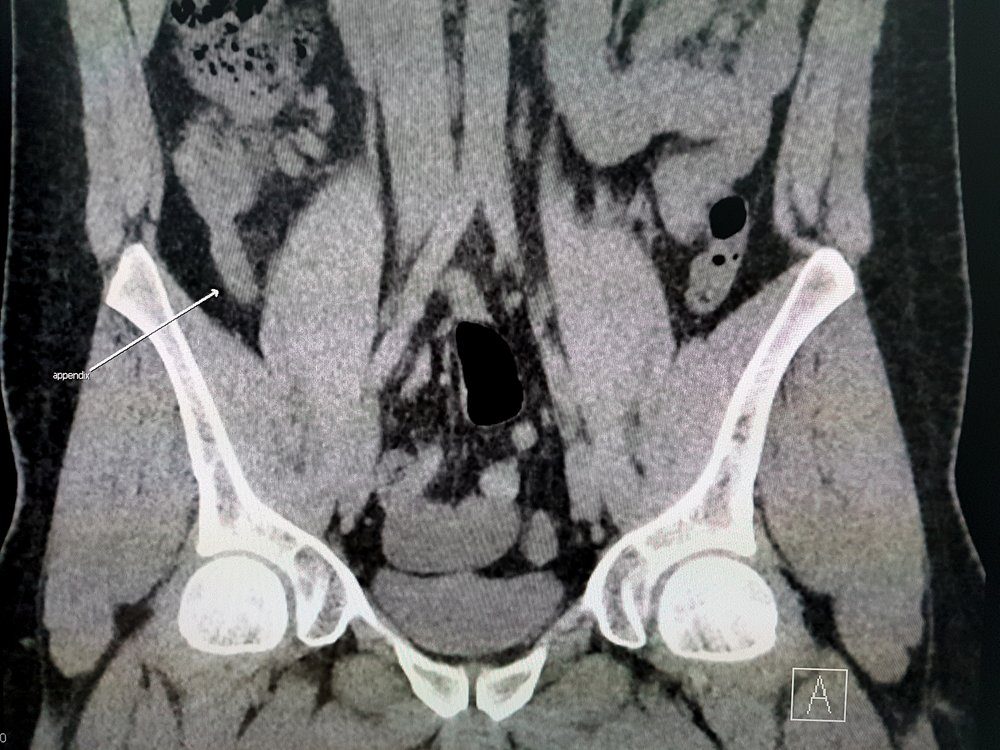
If you have a fever and you start to experience abdominal pain that starts around the belly button but within two hours moves to the right lower quadrant of the abdomen and becomes severe, those are signs you have appendicitis, says Dr. Nunziato-Ghobashy.
Appendicitis is typically confirmed with a CT scan and requires surgery to remove the appendix. If the surgery is not performed quickly enough, the appendix can burst and cause infection and even death.
These are the six appendicitis symptoms you need to watch out for.

Low back pain and blood in the urine
If you have a fever accompanied by burning pain when you urinate, lower back pain, pelvic pain, blood in the urine, or urine that looks cloudy or smells funny, says Dr. Nunziato-Ghobashy, you may have a urinary tract infection (UTI).
When such an infection gets bad, you’ll end up with a fever. Your doctor can take a urine sample to look for white blood cells, red blood cells, or bacteria—all signs of a UTI. Patients typically get medication for the pain as well as an antibiotic to eliminate the infection.
Here are 13 sexual health tips your urologist wants you to know.

Sore throat
Strep throat is a bacterial infection that’s more common in children than adults. It can cause an intensely sore throat along with a fever and, sometimes, a headache and nausea. “You need to be treated with antibiotics,” says Dr. Nunziato-Ghobashy. And you need to finish all the medication, even after your throat feels better, she warns. “Lingering strep bacteria can cause pericarditis, an infection of the heart valves, which is very serious.”
For a DIY sore throat remedy, here are 16 natural gargles for quick relief.
Digestive disorder
Irritable bowel syndrome, Crohn’s disease, ulcerative colitis and celiac disease all can trigger an inflammatory response in the body—and that can raise your temperature. “Sometimes fever is the first sign,” says Dr. Nunziato-Ghobashy. And if you alternate between constipation and diarrhea—common among patients with these disorders—the body can react to symptoms of dehydration and raise your temperature, she explains.
Don’t miss these easy ways to improve gut health.

Blood clot
Abnormal blood clotting—which prevents blood flow—is among the more dangerous symptoms to emerge in patients with severe COVID-19. But how exactly the coronavirus triggers the formation of blood clots is still a mystery.
One study, published in the journal Blood, suggests that changes in blood platelets triggered by COVID-19 may be to blame, possibly because that contributes to the onset of heart attacks, strokes, and other serious complications. The researchers found that inflammatory proteins produced during infection significantly altered the function of platelets, making them more prone to form potentially deadly blood clots in the lungs, as well as deep vein thromboses in the legs.
Whether caused by COVID-19 or not, “a deep venous thrombosis (DVT) is a serious medical condition that requires immediate care,” says Dr. LeRoy. “One of the signs of a DVT that is likely not present in COVID-19 would be a swollen, red, possibly tender leg where the blood clot had formed. Blood clots can sheer off and float to the lungs causing a pulmonary embolism—a clot trapped in a major lung vessel—which may cause severe chest pain along with trouble breathing. This can be life threatening and needs immediate medical attention.”
Here’s why some people are more likely to spread COVID-19 than others.

Joint pain
“Arthritis, especially rheumatoid arthritis, can raise inflammatory markers in the body and cause you to have fevers,” says Dr. Nunziato-Ghobashy. “Sometimes a fever that seems to have an unknown origin can be triggered by arthritis.” You may also have joint pain and body aches. Typically the pain will be felt on both sides of the body and is worse in the morning.
Discover the 30+ arthritis facts you need to know.
Breathlessness, exhaustion
Pneumonia inflames your lungs’ air sacs, which may then fill up with fluid or pus, according to the American Lung Association. The infection can be viral or bacterial. Symptoms, in addition to fever and chills, can include cough with mucus, chest pain, and shortness of breath. Always see a doctor if you suspect you have pneumonia, especially if you are in a high-risk group: children two or younger, adults 65 or older, and people with a chronic health condition or weakened immune system, and those who’ve been exposed to COVID-19.
“Fever, cough, and shortness of breath accompany both COVID-19 and pneumonia,” says Dr. LeRoy. “You should see your family physician if you have these three symptoms, regardless of exposure to Covid-19. When in doubt, check it out.”
Watch out for these 11 troubling new COVID-19 symptoms and complications.

Swollen neck, fatigue
Fever, fatigue, swollen lymph nodes in the neck, sore throat, and an enlarged spleen are the hallmark symptoms of Epstein-Barr virus, also known as mononucleosis. Common in childhood, less so among adults, it usually resolves in two to four weeks but can last for months, according to the Centers for Disease Control and Prevention. Your doctor can confirm the diagnosis with a blood test; treatment includes rest, drinking plenty of fluids, and taking OTC medications for pain and fever.
Try these eight natural ways to treat chronic fatigue symptom.

Skin infection
Cellulitis is a common—and serious—bacterial skin infection that often appears on the lower legs but can turn up anywhere on the body or face. It occurs when bacteria infect a break or crack in the skin; at first, you’ll see a swollen, red patch on the skin that is warm and painful to the touch. You may also get a fever, red spots, skin dimpling, and blisters. “The infection can spread quickly if not caught in time,” says Dr. Nunziato-Ghobashy. Seek emergency care if you notice signs of cellulitis.
Are you a hypochondriac? You might have Illness Anxiety Disorder.

The stomach flu
With gastroenteritis—commonly called the stomach flu—your digestive tract is irritated and inflamed, usually because of a bacterial infection, virus, or parasites. You may experience fever, nausea, chills, vomiting, stomach cramping, and loose stools. Symptoms typically last from two to 10 days and go away by themselves. But if you have been vomiting for longer than two days, you notice blood in your vomit or stool, or you have signs of dehydration, the Mayo Clinic advises seeing a doctor immediately. Infants, older adults, and people with compromised immune systems also need to see a doctor right away.
Here are 10 different stomach pains you shouldn’t ignore.

Cancer
A fever can accompany some cancers, including lymphoma, leukemia, and kidney and liver cancers. “They cause an inflammatory response in the body,” says Dr. Nunziato-Ghobashy. This is rare, she stresses, but something to pay attention to if you have a fever that persists. “If you can’t find a reason for your fever, it’s important to have somebody look to see professionally whether there is a reason.”
Next, here’s how to tell if your symptoms are COVID-19 or the flu.