The Trauma Room Black Box
Emergency-room doctors are not so different from the rest of us: they learn best from their own mistakes. But memories aren’t perfect—especially in high-stress situations—and the speed and complexity of what happens in a trauma room can make it hard to recall exact details. To remedy that, the trauma team at St. Michael’s Hospital in Toronto decided to take a cue from the aviation industry. They installed a black box in their trauma room, allowing them to later pinpoint an exact time when things went right—or started to fall apart.
“This is about reimagining trauma resuscitation so we can get factual feedback on performance,” says Dr. Chris Hicks, trauma physician who helped lead the project. The black box can record everything that happens using 360-degree cameras, wall-mounted microphones and connections to the patient’s vital signs. Once the team finishes working on a patient, doctors can review everything that happened—arming themselves with the skill and knowledge to work on the next trauma patient and, hopefully, save another life.
The Rise of Telehealth
Virtual health care has steadily gained traction in Canada since 2015, when Toronto emergency-room physician Brett Belchetz founded Maple, the country’s first national telemedicine platform. Three years later, Canadians completed over one million telehealth consultations—a 500 per cent jump in less than a decade. Unsurprisingly, the pandemic has further increased remote visits. In 2020, Maple added more than a million new patients and its consultation volumes tripled.
The platform is now open 24 hours a day, seven days a week and offers patients access to a doctor in two minutes or less. Patients can see a doctor either by video, instant message or phone call, depending on their needs—whether it’s an on-screen check-in with a family doctor or a virtual visit with a specialist. Such convenience raises the question: why would anybody want to return to the pre-pandemic system of crowded, boring waiting rooms? Luckily, now many of us won’t have to.
“Around 50 to 70 per cent of medical issues can be treated virtually, without a hands-on physical exam,” says Belchetz. Even better news: the pandemic has prompted some provincial governments, like B.C.’s, to cover the platform’s costs (it operates as a private, fee-based service). This new frontier of health-care delivery also promises to alleviate hospital staffing shortages and a lack of doctors in rural areas long after the COVID-19 pandemic.
Check out these tips on how take better care of yourself during tough times.
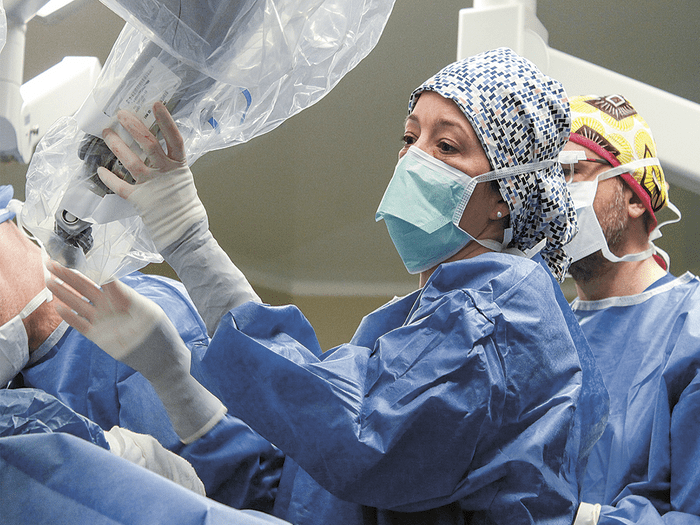
The Robot That Performs Mastectomies
Robot-assisted surgery offers patients the hope of smaller incisions, faster recovery and less noticeable scars. In November 2019, Toronto General Hospital received a new robot surgeon—a robotic arm that specializes in mastectomies, a first in Canada. And in February 2020, Dr. Tulin Cil, the hospital’s chair of breast surgery oncology, and her team became the first doctors to successfully perform a robot-assisted nipple-sparing mastectomy.
The use of the robotic arm assists in visualizing deeper into the breast, using a lens and a screen, and dissecting cancerous tissue from its healthy counterpart—enabling a patient to keep their nipple. (In typical mastectomies, the nipple is not spared at all.) The healing process is also faster with the nipple kept intact, allowing a patient to undergo immediate breast reconstruction and gain a more natural post-op appearance—a game changer for the one in eight Canadians who will experience breast cancer in their lifetime.
Don’t miss these five things you can do every day to prevent breast cancer.

The App That Manages Your Cancer Care
When Laurie Hendren was diagnosed with breast cancer in 2014, she assumed she’d have fast, up-to-date access to her test results and treatment plans. But she quickly discovered that this wasn’t the case: the process for viewing our own medical info is both challenging and time-consuming, involving several forms, a trek to the hospital’s medical records office and a wait of up to 30 days.
As a computer scientist, Hendren saw a better way: an app. She worked with doctors at McGill University Health Centre, where she was receiving treatment, to develop and launch Opal in 2019. The free app is customized for cancer patients and provides swift access to medical data, lab results, medical notes and treatment plans.
“This project was unique because it was led by Laurie,” says radiation oncologist Dr. Tarek Hijal. “The ideas came from her, and she vetted every step. Her insights are what made the end result so powerful.”
Sadly, Hendren died shortly after Opal’s launch, but her app is now used throughout the entire MUHC Cancer Centre, and plans are underway to bring it to hospitals across the country.
Here are 30 cancer symptoms you should never ignore.

The Drone That Delivers Emergency Supplies
Canada’s vast terrain makes it difficult—and in some cases impossible—to send urgent medicine and supplies to its most remote areas. InDro Robotics, a drone company based in Salt Spring Island, B.C., is set to change that. In August 2019, InDro pilots flew a drone carrying Narcan, an EpiPen and a prescription medication from London Drugs in Duncan, B.C., to three locations on Salt Spring Island. It was the first successful drone delivery of emergency medications over the Pacific Ocean. The 37-kilometre flight took only 11 minutes—saving enough time to make a critical difference.
The next month, the company partnered with Michael Nolan, chief of the Renfrew County paramedic service in rural Ontario, which serves an area of 7,250 square kilometres of densely forested, sparsely populated rural terrain. Nolan’s idea was to test how fast the drones could deliver a defibrillator. Several test flights were conducted, and each time, the drone arrived seven life-saving minutes earlier than the ambulance. Renfrew paramedics have since acquired a small fleet of drones, which they now use almost every day in their emergency services.
Thanks to these successes, the Canadian Transport Agency granted InDro Robotics the first commercial drone licence in the country in November 2020. Currently, the company is working on increasing their flight distance to 200 kilometres—potentially saving even more lives.
Read all about the 10 greatest Canadian health discoveries.

The Comfortable Hospital Bed
More than a quarter of Canadian patients develop pressure ulcers, or bedsores, from remaining in one position for too long during hospital stays. These wounds are tricky to treat and can increase the risk of sepsis and even death.
To combat this, four Ontario hospitals have tested swapping out their regular beds for ones that use artificial intelligence to gently move a person lying on them. The Swedish-made Ably bed, for example, predicts a patient’s movements and then uses adjustable longitudinal motion springs to redistribute their weight, significantly reducing the risk of sores.
These brainy beds can also help prevent falls: if an at-risk patient starts climbing out, sensors rearrange the bed into a bowl shape, providing extra seconds for a nurse or caregiver to arrive. The beds also monitor vital signs and will alert staff if a patient’s heart rate spikes or drops. Patients can expect to snuggle into a smart bed in the future as more hospitals make the switch.
Check out this COVID-19 patient’s incredible survival story.

The Virtual Care Assistant
Joyce Dingwell has lived at St. Joseph’s Continuing Care in Cornwall, Ont., for five years. As a small subacute care hospital, the facility rehabilitates patients who have experienced strokes and hip fractures, while also looking after long-term patients with conditions such as multiple sclerosis and ALS. At 82, Dingwell’s vision loss meant she relied on staff for everything from turning on the radio to phoning a friend. But what if, staff wondered, there was a simple fix to give her more independence?
In 2019, with the rise of voice-activated devices as their inspiration, staff headed to a nearby electronics store and bought a Google Home. The smart speaker connects to Google Assistant, which lets Dingwell use her voice to text, call, check her calendar, control her music, set timers, hear the weather, get the latest news and more. “It’s been so easy to figure out,” she says.
Buoyed by their success, staff next installed kits in the rooms of Liz Mullin and Scott MacIntyre, both of whom have MS. The first thing Mullin did was something she hadn’t done by herself in years: turn on her TV and change the channel. MacIntyre uses the device to control his room fan, lamp and television—all without calling the nurses for help. The staff now hopes to use what they’ve learned to help other long-term care facilities and hospitals set up voice-activated devices for their residents.
Read the inspiring story of how a Chicago hospital pulled off back-to-back triple organ transplants.

The VR Goggles That Improve Brain Surgery
For Canadians living with Parkinson’s disease, deep brain stimulation (DBS) can provide an entire decade of additional independent living. With DBS, a neurosurgeon places electrodes in a certain area of the brain, allowing it to receive impulses that remove or reduce tremors. The electrodes are controlled by a small generator placed in the patient’s chest. There’s only one hitch: for it to be effective, the placement must be precise, and each electrode is no thicker than a human hair. That can be difficult for even the most experienced surgeon to manage.
To help get it right, Dr. Adam Sachs, a neurosurgeon at the Ottawa Hospital, decided to try another up-and-coming medical innovation: 3-D virtual-reality tech. Usually, a neurosurgeon uses generic brain maps for DBS. But with a VR headset, Sachs can view and manipulate 3-D MRIs and CT scans of a patient’s own brain. This drastically improves precision and, thus, chances of success—like a fingerprint, our brains are unique to us, and even the smallest variances can make a big difference. While this approach is still under development, 3-D tech will likely be used in the future in every surgery imaginable.
Take a look at these healthy habits proven to boost brain health.

The Healing Powers of Art
Medical research has repeatedly shown that nature has powerful healing effects. One 2010 study, published in the Health Environments Research & Design Journal and conducted inside a simulated hospital patient room, found that seeing art and nature can relieve stress and pain by lowering both blood pressure and sensory pain responses. Unfortunately, most older hospitals have limited window views and few accessible outdoor spaces, making it difficult for patients to get those added healing benefits. That’s why some Canadian hospitals have decided to get creative.
In 2020, Kemptville District Hospital teamed up with a local photography club in Ontario to bring the therapeutic powers of nature into its hallways. Together, nurses and artists chose 20 large-scale nature images of recognizable regional landmarks. Next, they printed the soothing images on easily sanitized canvas and hung them in accessible hallways, where patients using wheelchairs or walkers pass by.
After the photos were installed, one elderly patient who was making slow progress toward recovery told staff she finally felt energized—she wanted to get out of the hospital so she could revisit the local landmarks herself.
Don’t miss out on the 15 benefits of walking for just 15 minutes a day.

The Doctors Who Listen
Traditionally, doctors learn about disease through textbooks and lectures—but rarely from patients themselves. Dr. Lynn Ashdown experienced this firsthand after an accident in 2014 left her paralyzed. In an instant, she went from being a doctor to being a patient and saw a stark contrast between her textbook knowledge and her actual experience. She decided to share her story to help other doctors bridge the physician-patient disconnect and, in turn, offer more informed care.
Since 2018, Ashdown has spoken at over 20 medical conferences and to thousands of health-care professionals, urging them to put patients’ experiences first. Today, she’s helping other patients learn how to improve their side of the conversation. Together with the Ottawa Hospital, Ashdown helped create a two-day storytelling workshop, teaching patients how to better voice their experiences of illness and disease. The first was held in October 2019, with 10 patients, and the program has continued online during the pandemic. She says many doctors have realized that care is too often done to the patient, not with them—and that needs to change.
Ashdown hopes to expand her workshop to other hospitals and, with it, the idea that doctors must listen to their patients more. “Sharing patient stories can give doctors a different view that would not otherwise be accessible to them,” she says. “It increases compassion and contributes to patient-centred care.”
Next, check out how a group of amateur hackers transformed diabetes care.